Liver cancer in adults
Summary
There are two types of liver cancer, primary cancer and secondary malignancies also called metastases.
Primary liver cancer is a malignant tumor that has developed from liver cells. The two most common types of primary liver cancer are hepatocellular carcinoma, the most frequent, and cholangiocarcinoma. Hepatocellular carcinoma, or hepatocarcinoma, represents 90% of primary liver cancers. It takes its name from the liver cells from which it develops, the hepatocytes. Cholangiocarcinoma is the second primary liver cancer, but this one develops from the cells of the bile ducts. It is very rare (about 420 cases/year in 2017). At the Cliniques universitaires Saint-Luc, approximately 50 patients were treated in 2019.
The liver can also be affected by metastases, which are tumors formed by cancer cells that have migrated from a tumor located elsewhere in the body (for example in the colon or breast). Colorectal cancer metastases are frequently found in the liver. Approximately 50% of patients with colorectal cancer will develop liver metastases. Half of them are present at the time of diagnosis of colorectal cancer, the other half may appear later. Tumors other than colorectal cancers can also induce metastasis in the liver (breast cancer, neuroendocrine tumors, etc.).
Risk factors
Most of the time, hepatocellular carcinoma occurs in a liver damaged by a disease (hepatitis or cirrhosis, often due to regular consumption of alcohol, hepatitis B and C viruses, or non-alcoholic steatohepatitis, "NASH"). It can also happen, rarely, that hepatocellular carcinoma develops in a person with a normal liver. As compared to hepatocarcinoma, cholangiocarcinoma more frequently develops in a liver that is not diseased. Thus, patients who have a small cancer may not be able to be treated properly because their liver is too damaged and no longer works well enough. Fortunately, improved liver function is regularly observed when people stop drinking alcohol, or when their virus is effectively treated.
Symptoms
Primary liver tumors are often discovered incidentally, for example during a follow-up ultrasound or in a patient with cirrhosis.
Treatments
All the patients presenting a malignant tumor of the liver are discussed in a multidisciplinary meeting (every week) where oncologists, radiotherapists, radiologists, anatomopathologists, nuclear medicine specialists, and surgeons meet to define the therapeutic strategy which will be proposed to each patient according to the type and extent of the tumor disease. Treatment options for primary cancers depend on the severity of the underlying liver disease and the extent of tumor in and outside the liver. Medical treatments depend on the extent of the cancer and include intra-arterial chemoembolization, radiofrequency, drug treatments, or radioembolization treatments. Surgical treatments include liver transplantation if liver disease is severe, tumor extension is limited (the criteria are strict), and there is no metastasis. Liver resections are indicated when the liver is normal (absence of cirrhosis) or slightly diseased and the tumor is resectable (removable) and in the absence of metastasis. The treatment of cholangiocarcinoma primarily depends on the stage of the tumor. Surgery is generally proposed when the patient has a tumor limited to one part of the liver and without metastasis. In other cases, chemotherapy is administered.
Treatments for liver metastases include chemotherapy, surgery, some radioembolization treatments, and radiation therapy.
Surgical treatments:
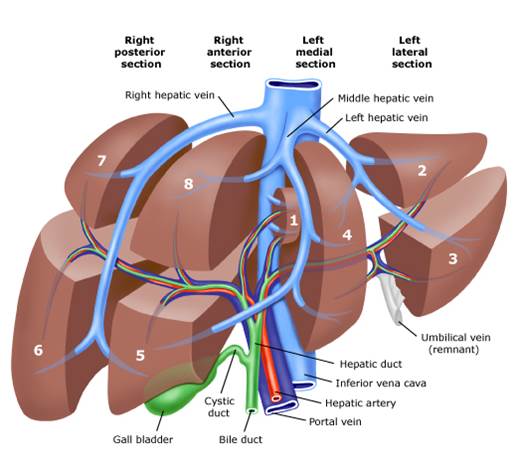
Surgical resections are often combined with chemotherapy when treating patients with colorectal cancers. Chemotherapy can be given before, after, or before and after surgery. The extent of surgical resection or type of hepatectomy will depend on the number and size of tumors to be removed. The operation can consist in removing only one of the 8 segments of the liver or up to 6 of the 8 segments. The most frequently performed major hepatectomies are right hepatectomy (taking segments V, VI, VII, and VIII), left hepatectomy (taking segments II, III, and IV), and extended right hepatectomy (taking segments IV to VIII).
These procedures are mostly performed as open surgeries (laparotomy). Conversely, a minor hepatectomy (which removes only 2 segments at most) can often be conducted by laparoscopy.
When a hepatectomy removing more than 4 segments of the liver is necessary, an interventional radiology technique called portal embolization is sometimes used to "enlarge" the liver that will remain in place after the resection if the volume is judged to be insufficient based on preoperative magnetic resonance imaging. Indeed, at least 30% of the total liver must be preserved after resection. Sometimes, when both sides of the liver are affected by metastases, two surgeries must be performed 2-3 months apart in order to remove all tumor lesions. During the preoperative consultation, the surgeon will explain the extent and type of liver resection to be performed as well as the technical details and possible complications that may arise.
Locoregional treatments:
Chemoembolization:
This is a treatment performed by radiologists, which consists of the highly targeted injection of small particles ("beads") loaded with chemotherapy into the liver, via the main artery of the liver (hepatic artery). This is an important treatment option for hepatocellular carcinoma (HCC). The particles are concentrated in the tumor(s), carried by the bloodstream to the tumor(s), which are usually very richly vascularized.
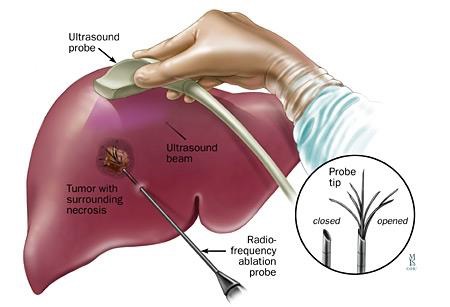
Radiofrequency:
Also performed by expert radiologists, this treatment is aimed at destroying the tumor (also most often a HCC) by heat. A probe is introduced into the liver through the skin and placed in the center of the tumor under ultrasound guidance; a current heats the probe up to 100°C, which allows complete and safe destruction of HCCs up to 2-3 cm in diameter.
Yttrium-90 radioembolization or selective internal radiation therapy (SIRT)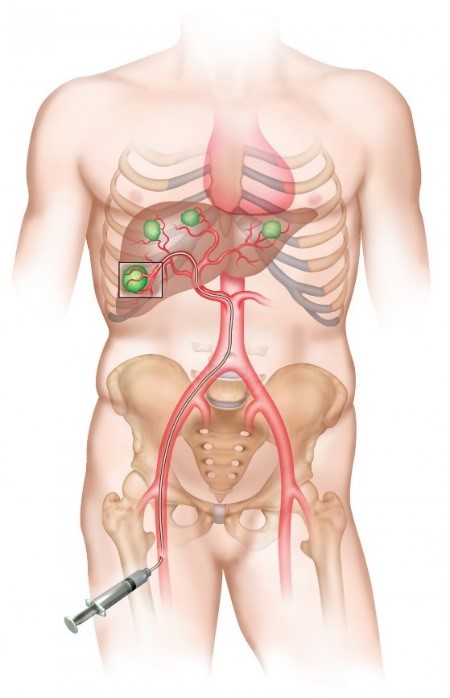
This treatment is proposed to patients with unresectable liver tumors (hepatocellular carcinoma, cholangiocarcinoma, or liver metastases).
The treatment is carried out by an interventional radiologist, through the injection of radioactive sources into the liver tumor(s). The radioactive elements (small-caliber microspheres loaded with Yttrium-90, considered as sealed micro-sources) that are concentrated in the tumors irradiate the cancerous cells while preserving the normal liver. Microspheres are delivered into liver tumors via the arterial network of the liver using a vascular catheter positioned by the interventional radiologist, under imaging guidance. Once the microspheres are implanted, they remain in place permanently and by its irradiating action on liver cancer tumors, this treatment slows down the evolution of the disease, and sometimes even reduces the size of the lesions and makes them operable.

Contact
For any further information, or if you would like to make an appointment, please contact the Oncology Care Coordinator at + 32 2 764 42 22 ou 78 82.
Doctor

Dr Laurence ANNET

Pr Selda AYDIN
Dr Eliano BONACCORSI

Pr Ivan BORBATH

Pr Olga CICCARELLI

Dr Laurent COUBEAU
Pr Géraldine DAHLQVIST

Dr Astrid DE CUYPER
Pr Bénédicte DELIRE

Pr Pierre H. DEPREZ

Dr Cristina Anca DRAGEAN

Pr Catherine HUBERT

Pr Nicolas LANTHIER

Pr Renaud LHOMMEL
Dr Lancelot MARIQUE

Pr Peter STARKEL

Dr Pierre TREFOIS

Pr Marc VAN DEN EYNDE

Dr Sandy VAN NIEUWENHOVE

Pr Geneviève VAN OOTEGHEM
Paramedical
Laurie de BASSOMPIERRE

Marianne DEMORCY

Tuan LE TRONG

Annie MOREL
Laura THONET
Stéphanie TORDOIR


