Ocular cancer
Each European country has a reference center for ocular oncology. Our Ocular Oncology Unit has acquired major experience in the treatment of ocular cancers, which is internationally recognized. The vast majority of cases of ocular melanoma observed in Belgium are therefore referred to the Ocular Oncology Unit, as is retinoblastoma, the most frequent cancer of the eye in children (1 case / 20,000 births). The Ocular Oncology Unit also receives patients from several neighboring countries.
Retinoblastoma in children HERESummary/Epidemiology
Melanoma is the most common ocular cancer in adults. Its annual incidence in Belgium is approximately 7 to 8 new cases per million inhabitants. It has not changed over the last 20 years.
Risk factors
No factor that would favor the occurrence of ocular melanoma has been identified so far, although the majority of them develop from a suspicious nevus or "mole". The average age of onset of the disease is 60-65 years..
Symptoms
Intraocular melanoma is often discovered incidentally. By originating in the choroid (the vascular layer under the retina), it causes a detachment of the retina and can therefore lead to vision problems. However, these are not specific to cancer and can be found in many other diseases.
Diagnosis
The treatment of patients with ocular melanoma is determined at multidisciplinary meetings attended by ophthalmologists, radiotherapists, medical oncologists, and pathologists. The optimal attitude is then defined, according to the characteristics of the tumor, on the basis of the most recent knowledge. It is crucial to diagnose ocular melanoma at an early stage: timely identification of the lesion greatly increases the likelihood of therapeutic success.
Examinations
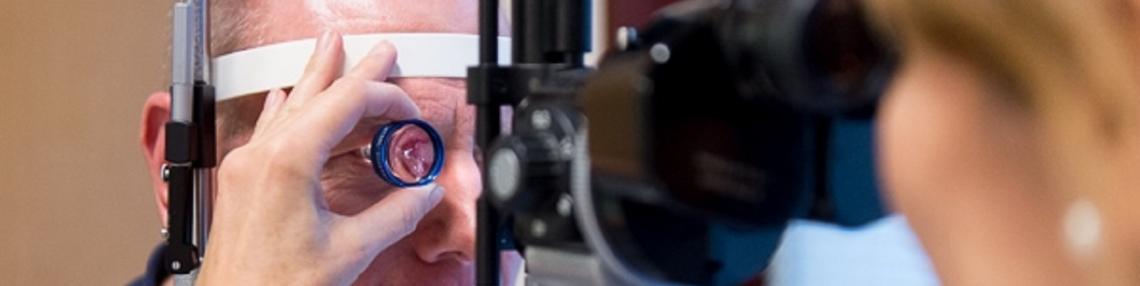
The diagnosis of intraocular melanoma is made during an examination called fundus, which allows the retina and choroid to be visualized through the dilated pupil. This diagnosis requires a certain amount of practice: it is not always easy to recognize a suspicious "mole". The so-called "ophthalmoscopic" image, observed with the naked eye, and imaging techniques, particularly ultrasound and magnetic resonance, allow the diagnosis to be confirmed in 99% of cases. Biopsy is rarely required.
Needle biopsy, performed under local anesthesia, is sometimes part of a research program to study the behavior of cancer and to identify certain genetic features of the tumor that would have a prognostic impact.
Treatments
Treatment is initiated within one week of diagnosis. New techniques have been developed in recent years. In most cases, they allow the eye to be preserved and avoid enucleation (surgical removal of the eye).
Transpupillary thermotherapy consists of inducing a temperature in the tissues that is higher than 45°C and lower than 60°C in order to kill the melanoma cells. A laser beam passes through the pupil and is focused on the tumor. This technique is used on an outpatient basis and does not require hospitalization or surgery. Transpupillary thermotherapy sessions can be repeated if necessary. The therapeutic success rate obtained in the Ocular Oncology Unit of the King Albert II Institute reaches 94%.
Contact radiotherapy offers a comfortable alternative to enucleation surgery when the size and location of the ocular melanoma does not allow for transpupillary thermotherapy to be performed. Contact radiotherapy, or brachytherapy, consists of placing radioactive seeds (Iodine 125) glued to a support plate on the ocular surface in contact with the tumor for 3 to 4 days during a surgical procedure. In Belgium, this very specific cutting-edge technique is only available at the Ocular Oncology Unit of the King Albert II Institute.
Contact radiotherapy can control the tumor in 97% of patients. However, in 5 to 10% of cases, it can lead to various complications that ultimately require enucleation. Sometimes contact radiotherapy is combined with transpupillary thermotherapy to increase the therapeutic success rate.
The chances of preserving useful vision at the end of these treatments depend mainly on the size of the tumor and its location in relation to the optic nerve and the macula (central area of the retina).
Enucleation remains the only option when the tumor is too large to be effectively treated by any other approach.
The advances made in the local treatment of ocular melanoma do not always prevent the occurrence of distant recurrences, most often in the liver. These metastases darken the prognosis. The research undertaken at the Ocular Oncology Unit therefore focuses on "adjuvant" treatments which, given in addition to local treatment of the tumor, aim to reduce the risk of metastasis.
Research / Innovation
The characteristic of ocular melanoma recurrence is that it is most often localized exclusively to the liver. If it is unique then local treatments can be proposed such as surgery, radiofrequency, or radioembolization. Unfortunately, most of the time, the recurrence is multifocal and these treatments are no longer possible to control the disease, so systemic treatments must be administered. While chemotherapy and targeted therapies are not very effective, immunotherapy gives patients more hope. Our group has made a significant contribution to the advancement of immunotherapy. We all have lymphocytes that can recognize and destroy tumors. However, anti-tumor lymphocytes fail to kill the tumor in many patients. Analysis of the mechanisms of resistance to the immune system has identified several mechanisms. Lymphocytes are very powerful weapons that are tightly controlled. Two regulation mechanisms have been identified: CTLA-4 / B7 and PD-1 / PD-L1 interaction. Antibodies blocking these interactions have been developed and successfully tested in patients with various cancers. Ipilimumab is an antibody directed against CTLA-4 that restores and prolongs the activation of T lymphocytes. It is administered intravenously every 3 weeks and the adverse effects observed are an overactivation of the immune system leading to autoimmune diseases. Some patients show sustained responses. Anti-PD-1 antibodies, such as pembrolizumab and nivolumab, have almost the same mode of action but are more effective and less toxic. In clinical trials, we are trying to further improve these results by combining different drugs that modulate the immune system in patients with metastatic melanoma.
Contact
For any further information, or if you would like to make an appointment, please contact the Oncology Care Coordinator at + 32 2 764 35 12.
Doctor

Dr Paulina BARTOSZEK

Pr Jean-Francois BAURAIN

Dr Frank CORNELIS

Dr Dario DI PERRI
Dr Eléonore LONGTON

Pr Geneviève VAN OOTEGHEM
Paramedical

Louise FAVARETTO

Florence FONTAINE

Amélie HOCEPIED

