Testicular cancer

Summary/Epidemiology
The testicles are located in the scrotum; they are the place where testosterone (the male hormone) and sperm are produced. Less than 500 cases of testicular cancer are diagnosed each year in Belgium; it is therefore a rare cancer, but it is the most common malignancy in young adults and most often appears between the ages of 20 and 40.
The main risk factor is cryptorchidism, which is a late and incomplete descent of one of the two testicles.
There are two types of testicular cancer, defined based on anatomopathological examinations: seminoma and non-seminoma cancers. This distinction is important because it determines the treatment, monitoring, and prognosis.
Symptoms and diagnosis
The most common symptom is swelling and/or pain in one of the two testicles. Any testicular swelling remains a diagnostic emergency and should be investigated.
A testicular ultrasound is performed to identify any testicular abnormality. If cancer is suspected, surgery will be performed (orchiectomy) to resect the testicle. Anatomopathological examination is important to distinguish a seminomatous tumor from a non-seminomatous tumor. A blood test will also evaluate different proteins that may be produced by the cancer cells; these proteins are not always present in the blood, but when they are, their evolution (decrease or increase) enables to judge the response to treatment
Treatment
The testicular cancer cure rate is high, but the disease still requires multidisciplinary management.
Testicular cancer usually requires resection of the affected testicle (orchiectomy). An imaging assessment must always complete this procedure.
- In the absence of lymph nodes or distant suspicious lesions, surveillance after orchiectomy is necessary, but in cases with a high risk of recurrence, chemotherapy can sometimes be proposed to reduce the risk of disease recurrence.
- In case of lymph nodes or metastases, chemotherapy will be proposed. This chemotherapy consists of the administration of several molecules (BEP = Bleomycin, Etoposide, Platinum), administered intravenously in hospital. Radiotherapy may sometimes be proposed in case of a single lymph node.
The choice of these treatments will be discussed in a multidisciplinary oncology consultation (MOC) where the different experts of our center will meet. These treatments all have their own adverse effects, which will be explained by the physician involved.
It is worth noting that even testicular cancer with metastases can be cured with the proposed treatments. Since the treatment involves the genital organs that produce sperm, sperm cryopreservation is performed before chemotherapy or radiotherapy.
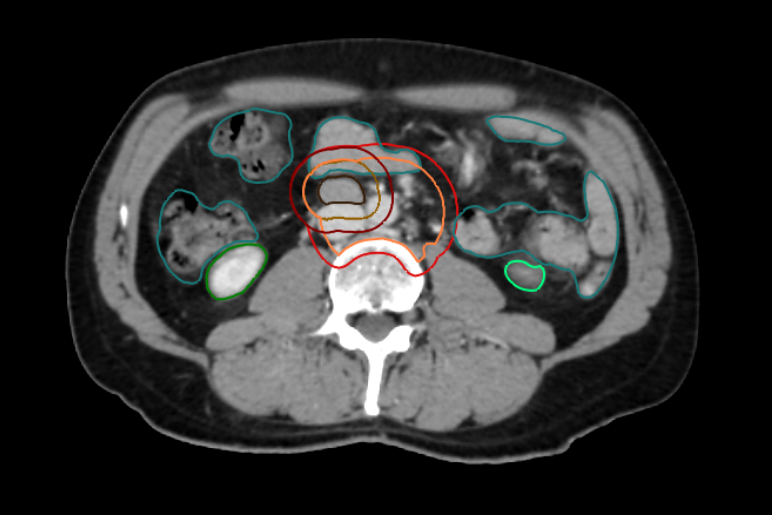
Through medical research, we continue to refine our diagnostic and treatment methods. In our institution, we evaluate different types of imaging techniques, in particular whole-body magnetic resonance imaging which, in addition to combining several examinations at the same time, makes it possible to specify the presence or location of suspicious lesions. As a center of expertise, we continue to study this cancer, in collaboration with world-renowned centers, in order to offer patients the best diagnostic and therapeutic strategy.
Contact
For any further information, or if you would like to make an appointment, please contact the Oncology Care Coordinator at + 32 2 764 35 44.
Doctor

Dr Laurence ANNET

Dr Hélène DANO

Dr Axel FEYAERTS

Pr Jean-Luc GALA

Dr Marco GIZZI

Dr Sofie HEYLEN

Pr François JAMAR

Pr Fréderic E. LECOUVET

Pr Renaud LHOMMEL

Pr Jean-Pascal MACHIELS

Pr Vassiliki PASOGLOU
Dr Barbara SCHMIDT
Pr Emmanuel SERONT

Dr Stéphane THIRY

Pr Bertrand TOMBAL

Dr Julien VAN DAMME

Dr Sandy VAN NIEUWENHOVE

Dr Ad VANDERMEULEN
Paramedical

Karoline AMANN

Naila EL IDRISSI

Kim HENQUIN

Monique KASA VUBU

Christine REMACLE

