Pancreatic cancer in adults
Summary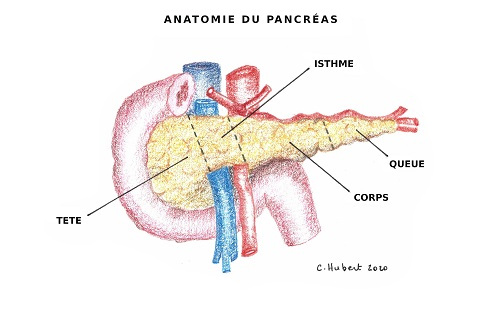
The pancreas consists of several parts: the head, the isthmus, the body, and the tail.
The most common type of pancreatic cancer is the adenocarcinoma. It is a rare tumor that occurs in 1–10 per 100,000 inhabitants.
There are also tumors of the pancreaticobiliary junction, which include cancers of the head of the pancreas, the duodenum, the ampulla (ampulloma), and the intra-pancreatic bile duct.
Risk factors
The main risk factors are smoking, diabetes, obesity, and chronic pancreatitis.
Symptoms
Symptoms are usually weight loss, abdominal pain, fatigue, loss of appetite, the occurrence of diabetes, and jaundice (this last symptom occurs only if the tumor is located in the head of the pancreas).
Examinations
When a tumor is discovered in the pancreas, additional examinations are carried out (CT scan, echo-endoscopy with biopsy, PET-CT) in order to stage the tumor.
Treatments
Cases are always discussed in a multidisciplinary meeting with a group of experts from each specialty who will determine the most appropriate treatment depending on the extent of the disease.
There are basically three possible scenarios:
If the tumor has metastasized, the treatment of choice will be chemotherapy. The patient will meet with an oncologist who will explain the type of chemotherapy he or she proposes to administer, the treatment modalities, and the adverse effects of the treatment.
If the tumor is "locally advanced", usually because it is in contact with large digestive vessels, then neoadjuvant therapy is proposed. This is an "attack" treatment that is aimed at shrinking the tumor so that it becomes operable. The treatment consists of chemotherapy and sometimes chemotherapy followed by radiotherapy.
If the tumor is immediately operable, surgery is proposed. The patient is seen in consultation by a surgeon who will explain the details of the operation, the possible complications, the length of hospitalization, etc.
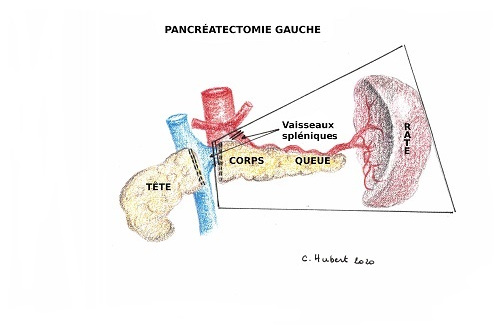
The surgical intervention will be very different depending on whether the tumor is located in the head and isthmus of the pancreas (right part of the pancreas) or in the body or tail of the pancreas (left part).
Tumors located on the left side can be excised by removing the body and tail of the pancreas and sometimes the spleen (splenectomy). This procedure, which is moderately complex, can be performed in the vast majority of cases by laparoscopy (small holes and camera).
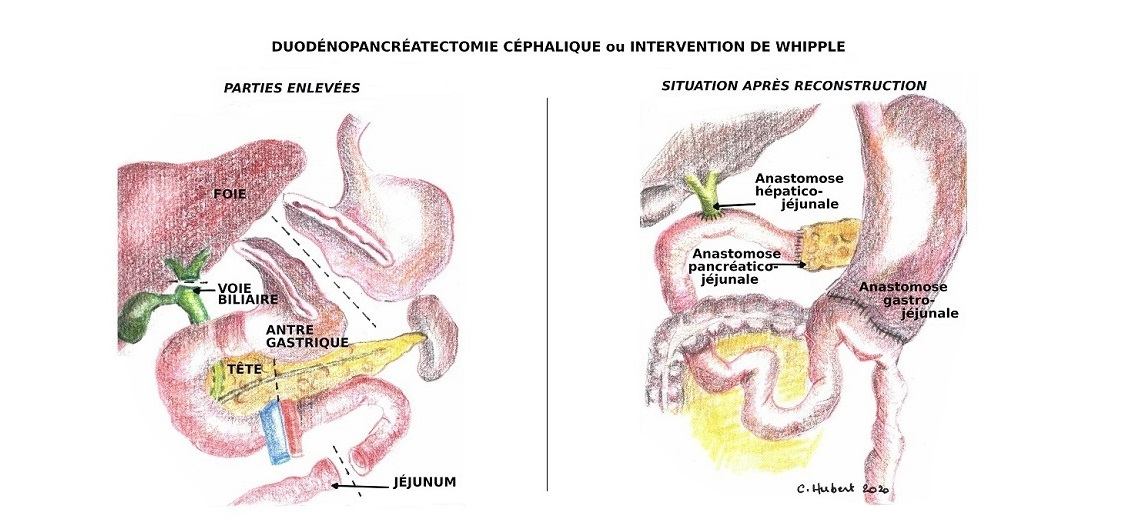
Conversely, tumors located in the head of the pancreas, as well as other tumors of the pancreaticobiliary junction, will require a much more extensive operation, which is called cephalic pancreaticoduodenectomy or Whipple procedure (named after the surgeon who performed this operation for the first time in 1935).
As the head of the pancreas is nestled in the curve of the duodenum and is crossed by the bile duct, it is not possible to remove only the head of the pancreas. The Whipple procedure consists in the removal of the duodenum, part of the stomach, the first 15 centimeters of the small intestine, the bile duct, and the gallbladder. It is then necessary to make a reconstruction of the digestive system requiring several anastomoses.
During the consultation, the surgeon will detail all these technical aspects and the surgical follow-up.
Contact
For any further information, or if you would like to make an appointment, please contact the Oncology Care Coordinator at + 32 2 764 42 22 ou 78 82.
Doctor

Dr Laurence ANNET

Pr Selda AYDIN
Dr Eliano BONACCORSI

Pr Ivan BORBATH

Pr Olga CICCARELLI

Dr Laurent COUBEAU
Pr Géraldine DAHLQVIST

Dr Astrid DE CUYPER
Pr Bénédicte DELIRE

Pr Pierre H. DEPREZ

Dr Cristina Anca DRAGEAN

Pr Catherine HUBERT

Pr Nicolas LANTHIER

Pr Renaud LHOMMEL
Dr Lancelot MARIQUE

Pr Peter STARKEL

Dr Pierre TREFOIS

Pr Marc VAN DEN EYNDE

Dr Sandy VAN NIEUWENHOVE

Pr Geneviève VAN OOTEGHEM
Paramedical
Laurie de BASSOMPIERRE

Marianne DEMORCY

Tuan LE TRONG

Annie MOREL
Laura THONET
Stéphanie TORDOIR

